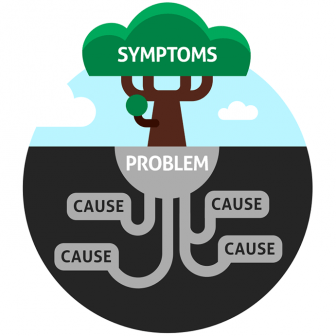
Is there ever one cause or cure for IBS?
 Is it human nature? Do there always need to be a single ’cause’ for illness? Can we just not get our heads around anything more complicated? Is it part of our culture of blame? Do we have to point the finger at someone or something?
Is it human nature? Do there always need to be a single ’cause’ for illness? Can we just not get our heads around anything more complicated? Is it part of our culture of blame? Do we have to point the finger at someone or something?
The notion of illness as having a specific cause, a definite diagnosis and a single effective cure is a throwback to the pandemics of infectious disease. For syphilis, tuberculosis, malaria, pneumonia, smallpox and many other communicable diseases, there was an identifiable micro-organism and antibiotics and immunisation cured or eradicated the disease. These days it is not like that.
Disease requires a combination of factors. Even with infections, not everybody gets ill. People differ in their resistance to infection. Malnutrition, stress, genetics, fatigue, the commensal bacteria that live on or within our bodies, may weaken a person’s constitution to such a degree that a super-added infection may tip it over into a cascade of disease.
It is the same with politics, where culture, history, climate, economics, deprivation, inequality come together to create a sense of grievance and then something happens; the harvest fails, or somebody gets killed and suddenly you have a revolution or war. We could speculate as to how much the ubiquity of social media exaggerates these effects and foments crisis? But that’s another story.
So what is it with IBS? Despite decades of research, nobody has really come up with a definitive cause or even a pathological mechanism. A major part of the problem is that the nature of IBS has never been accurately defined. The efforts of successive Rome committees have only succeeded in defining what it isn’t. A positive diagnosis has always seemed an illusion. Nevertheless, research has come up with some important insights. These include studies that appear to show that small intestinal bacterial overgrowth might cause symptoms that resemble IBS, that consumption of poorly absorbed sugars (FODMAPs) can provoke symptoms of diarrhoea and bloating in some people, that an attack of gastroenteritis may persistent symptoms of abdominal discomfort and bowel upset in about 15% of people and that many people reported that the onset of their IBS follows an episode of trauma.
Other research, mainly carried out in diarrhoea-predominant IBS, indicates a combination of factors that could induce disease. They include: an increase in intestinal permeability, immune hyper-reactivity, depletion of the colonic microbiome, alterations in neurotransmitters in the enteric nerves, changes in the brain gut axis and psychological tension. Which of these might be causes and which effects is unclear and probably irrelevant. It would seem more realistic to regard the irritable gut as a system of interconnected abnormalities that reset the gut to a more sensitive state. There are many routes to the same diagnosis and the degree to which different factors are important may differ from person to person. This systemic approach to understanding IBS would explain why the illness can wax and wane as the influence of various factors fluctuate. For example, food intolerance can vary according to what is happening in a person’s life; immunological factors may determine whether stress causes disease in the gut or the skin or any other organ.
The multifactorial nature of IBS also explains why a single treatment doesn’t always work. A low FODMAP diet doesn’t work for everyone, and it should not be a diet for life. There are other factors involved and life may change. Rifaximin, hypnotherapy, colonic irrigation, probiotics may help some of the people with IBS some of the time, but none should be regarded as a cure. They may just act to tip the balance of factors to one that is less irritating for a while.
But there is another concern. Any intervention in an illness system like IBS will have knock on effects that may not always be beneficial. For example, recent studies have shown that FODMAP exclusion can deplete populations of bifidobacteria and may lead to detrimental changes in permeability and immune reactivity, creating a sensitivity that might require more extreme FODMAP exclusion. There might also be questions about treatment of suspected small intestinal bacterial overgrowth with the poorly absorbed antibiotic, Rifaximin. Since the antibiotic Rifaximin is soluble in bile, it has been claimed that it will only eradicate those bacteria growing in the small intestine. But many people with IBS-diarrhoea have bile acid malabsorption, creating conditions whereby Rifaximin dissolved in unabsorbed bile could decimate the fermentative bacteria in the colon. While this might reduce gas production and symptoms in the short term; the longer term effects could be an increase in colonic sensitivity due to bacterial depletion. Such examples caution doctors and dietitians should intervene in systems like IBS advisedly.
It is often better to use a holistic approach to boost a person’s resilience and induce healing. This would include adopting a healthy life diet and life style, reducing intake of fatty food, alcohol, hot spices, onions, fruit and pulses, getting sufficient rest and sleep, adequate exercise and avoiding those situations that are particularly stressful. Activities that induce a state of mindfulness, complementary therapies, counselling or psychotherapy to help people understand and manage those situations that upset their gut, are particularly useful. Antispasmodics, antidiarrhoeal drugs, laxatives, and FODMAP exclusion may be useful for a while to suppress symptoms but should not be regarded as long term treatments. It would seem better to calm and heal the irritable gut than suppress it.

Pingback: The Fallacies and Fallibilities of IBS Research. | The Sensitive Gut
Pingback: ME/CFS and IBS: Are they two sides of the same coin? | The Sensitive Gut
Pingback: Loose Joints and Irritable Bowels; What’s the Connection? | The Sensitive Gut