IBS: more than just a pain in the neck.
So why haven’t we thought of it before? Intrigued as to why joint hyper-mobility or Ehlers Danlos Syndrome (EDS) might be associated with migraine, IBS and a whole variety of unexplained diseases. I asked my colleague, Professor Yan Yiannakou, research gastroenterologist at the County Durham and Darlington NHS Trust. Yan told me of some recent research that indicated that EDS (hyper-mobility type), an illness that affects the connective tissue of ligaments and tendons, might not only cause double jointedness, bunions, flat feet and arthritis, it could also cause instability of spinal cord supporting the skull. This could affect the brain stem autonomic (sympathetic and parasympathetic) nuclei responsible for controlling the function of viscera throughout the body, notably heart rhythm and rate, bladder tone, vascular constriction and blood flow and of course, the motility and secretion of the gastrointestinal tract.
It might be another explanation as to why IBS is associated with a variety of other unexplained syndromes, such as chronic fatigue, migraine, indigestion, bladder dysfunction. Temporo-Mandibular joint dysfunction (jaw dislocation and clicking jaw) is also a feature of EDS and associated with IBS.
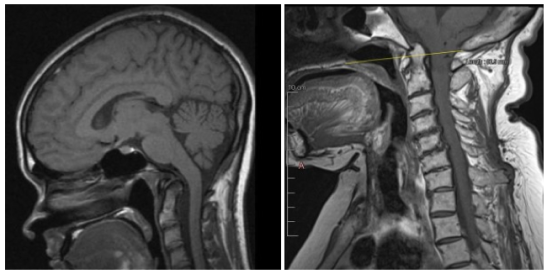
Looking further into this, the link between EDS and ‘autonomic syndromes’ is more likely if patients also have what is known as the Chiari malformation where the brain stem herniates through the foramen magnum and is squeezed by the upper spinal canal. Chairs malformation is found in about one in a thousand people. Mechanical distortion may not be the only explanation for autonomic stimulation; an unstable neck would constrict the flow through the vertebra-basilar arteries which supply blood to the brain stem.
EDS is not a common condition. It is said to be found in 1 in ten thousand people, though some doctors think it is much more common. But, I wondered, could the autonomic nuclei in the brain stem also be affected by whiplash injury to the neck? Some patients relate the onset of their IBS to a car accident. I had always tended to think this was due to the psychological trauma, but it may not be, though the of course the combination of physical and psychological trauma may well summate. Illness is rarely related to a single causal mechanism.
A brief enquiry of Google Scholar revealed a paper by another of my colleagues, Dr Anton Emmanuel, a neuro-gastroenterologist at University College London and the Hospital for Nervous Diseases at Queen’s Square. It was he and his research fellow, Dr Chung, who wrote a review identifying how common IBS and other unexplained illnesses affecting the gut, are after injury to the neck, and how symptoms could go on for years. Another recent paper showed that about 15% of people with a history of whiplash injury have herniation of brain stem into the spinal cord, though there was no comment as to whether this could have been secondary to the injury.
As far as treatment is concerned, some have claimed good results from a procedure known as prolotherapy, in which irritant solutions are injected into the neck to tighten up the connective tissue, but there is no substantive research to prove its efficacy, though more severe symptoms may benefit from cervical spinal fusion.

Could it just be that the Vagus nerve is affected, and in turn leads to a diverse of IBS issues?
LikeLike
Yes certainly, but instability of the neck could affect the dorsal vagal nucleus.
LikeLiked by 1 person